What is telemedicine?
The term telemedicine is an innovative form of medical care. Health services, diagnoses and treatments are carried out via digital communication media. Physicians can easily use their computer or smartphone for remote medical treatment without the need for the patient to be physically present. The spectrum of telemedicine includes video phone calls as well as simple text messages and emails. Several providers have specialized in providing telemedicine platforms that are intended to simplify communication.
How have telemedicine treatments developed?
The development of remote medical treatment actually dates back to the 1960s. The first milestones for today's telemedicine were set here:
- Start of remote treatments: NASA laid the foundations for telemedicine in the 1960s: It developed various systems to be able to check the health of its astronauts in space.
- Technological progress: In the 1970s, more and more companies specialized in the development of telemedicine systems. With the advent of the Internet and digitalization in the 1990s, telemedicine technologies continued to develop. The use of emails, video conferences, and digital image transfers became more and more common.
- COVID-19 pandemic: The corona pandemic in 2020 led to a huge boost in the use of telemedicine. Lockdowns and social distancing increased demand for virtual doctor visits and accelerated the integration of telemedicine into healthcare worldwide.
- Regulatory changes: Many laws and regulations have been amended to facilitate the use of telemedicine. This includes recognizing online consultations, reimbursing for telemedicine services, and ensuring the security of patient data.

Benefits of remote medical treatment
Many doctors are wondering whether you should offer telemedicine in your practice. The following points speak in favour of providing the service:
Improved accessibility
Rural areas in particular benefit from improved accessibility and accessibility of medical services. There is an acute shortage of doctors in rural areas of the Federal Republic of Germany, and there are also mobility problems among patients due to their age or chronic illnesses. Thanks to telemedicine, these patients can access a consultation with a doctor very quickly without having to travel long distances. But doctors can also use their resources more effectively and no longer have to make complex home visits for certain matters, for example.
Reducing waiting times
Long waiting times in doctors' offices and clinics are a common nuisance. Telehealth enables more flexible scheduling: Since virtual consultations are less time-consuming than physical doctor visits, more appointments can be offered in a shorter period of time, resulting in shorter waiting times. This enables more efficient use of time for both patients and medical staff and contributes to faster diagnosis and treatment.
cost savings
The use of telemedicine can result in a significant reduction in costs. Patients save on travel and parking costs. But the healthcare system is also benefiting, as remote treatment, for example, can reduce workload in medical practices. This allows the already scarce staff to be used more effectively, which saves costs.
What treatments is telemedicine suitable for?
- Check-ups: Telemedicine is particularly suitable for patients who want to undergo a routine examination. This includes discussing laboratory results, medical advice or testing medications. This allows doctors to review medication plans, make adjustments, and monitor patients' progress.
- Chronic disease management: Telehealth is ideal for managing chronic diseases such as diabetes, high blood pressure, or heart failure. Patients with certain health conditions can be monitored from home, for example when monitoring blood sugar levels, blood pressure, or heart rate. Physicians can analyse this data and intervene when needed.
- Psychiatric care: Telepsychiatry also enables the remote treatment of mental health problems. Therapeutic sessions, counseling, and medication management can be easily delivered via video conferencing.

When on-site testing should be preferred
However, not all medical situations are suitable for telemedicine. Acute emergencies or cases that require a physical examination are still better suited to traditional medical visits. Furthermore, complex or unclear clinical patterns should also be examined on site, as extensive diagnostic tests are required here in order to be able to make an accurate diagnosis. An incorrect diagnosis via remote treatment could therefore lead to enormous health risks.
Ultimately, treating doctors must be able to decide when they can make good use of telemedicine and when treatment is needed in practice.
What do doctors have to consider when offering digital consultations?
Physicians who want to offer telehealth in their practice should consider several aspects to ensure that virtual consultations are effective, ethical, and safe:
- Privacy and security: Physicians must ensure that the platforms they use for digital consultations meet strict data protection standards. Patient data should be transferred and stored securely. The Federal Association of Statutory Health Insurance Physicians (KBV) provides a Directive on requirements for ensuring IT security ready.
- Approval: Physicians should ensure that they have the necessary licenses and approvals to offer telehealth in their region. The legal requirements may vary by country or state. As a rule, a electronic medical profession card (eHBA) necessary.
- Patient education: It is important to educate patients about the process, technology and limitations of digital consultations. Eine successful doctor-patient communication is all the more important for treatment success virtually.
- documentation: Physicians should document digital consultations as well as physical visits. This includes diagnoses, treatment plans, prescribed medications, and other relevant information. Comprehensive documentation is important for the continuity of patient care.
- Billing and compensation: Clarify in advance how digital consultations are billed and which insurance covers them. Clear communication with patients about billing modalities is important.
The future of the healthcare system is digital
Overall, telemedicine care outside practice should be made even easier in the future. The representative meeting of This year, KBV has adopted key points and defined framework conditions. Corresponding regulations are now being negotiated with health insurance companies and are to be enshrined in the Federal Coat Contract Physicians and in the Uniform Assessment Standard (EBM).
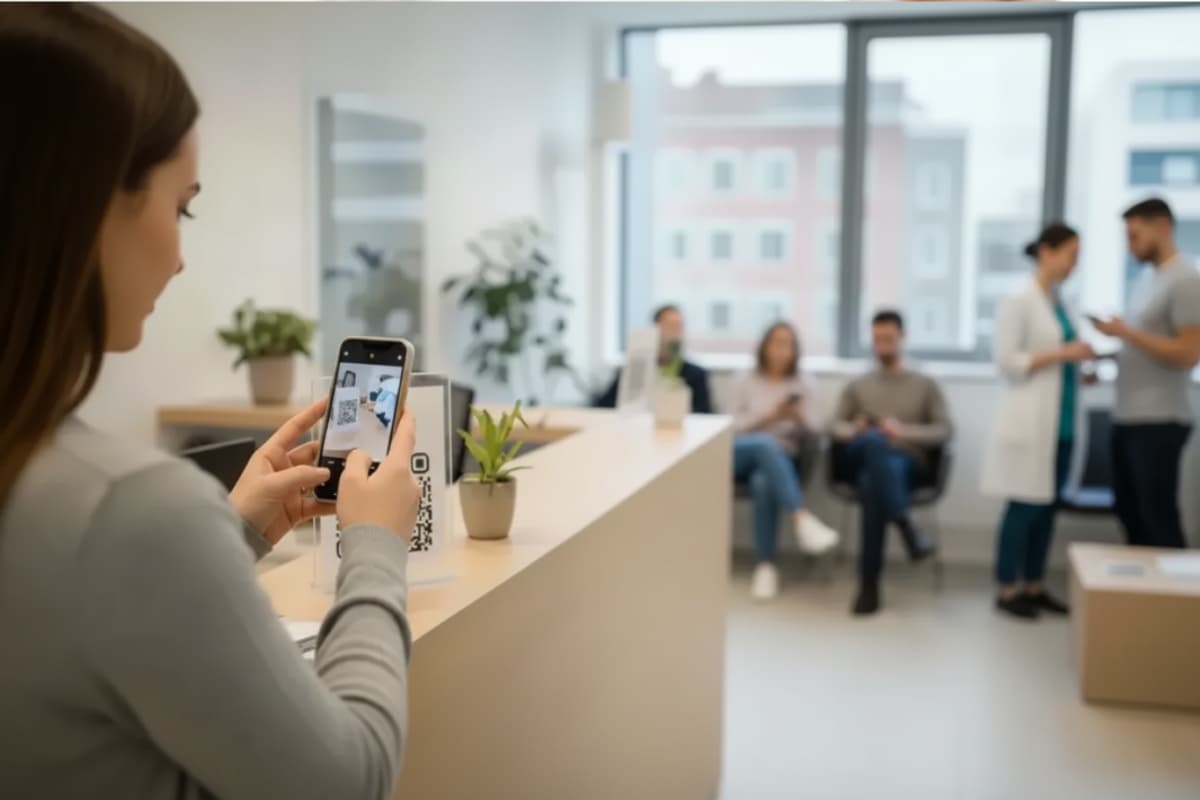
This development makes it clear that the healthcare system in Germany is on the way to becoming ever more digital. Nelly also steps in here: Regardless of digital patient recording, simple document management or convenient payment processing — With Nelly, a digital practice routine can be created. Practice saves resources, gains efficiency and benefits from modern communication channels. Sounds interesting? Wir advise you without obligation and free of charge to your individual case!
Contact Nelly now!
The personal names used in this article always refer equally to all persons. Dual naming and alternate names are omitted in order to improve readability.